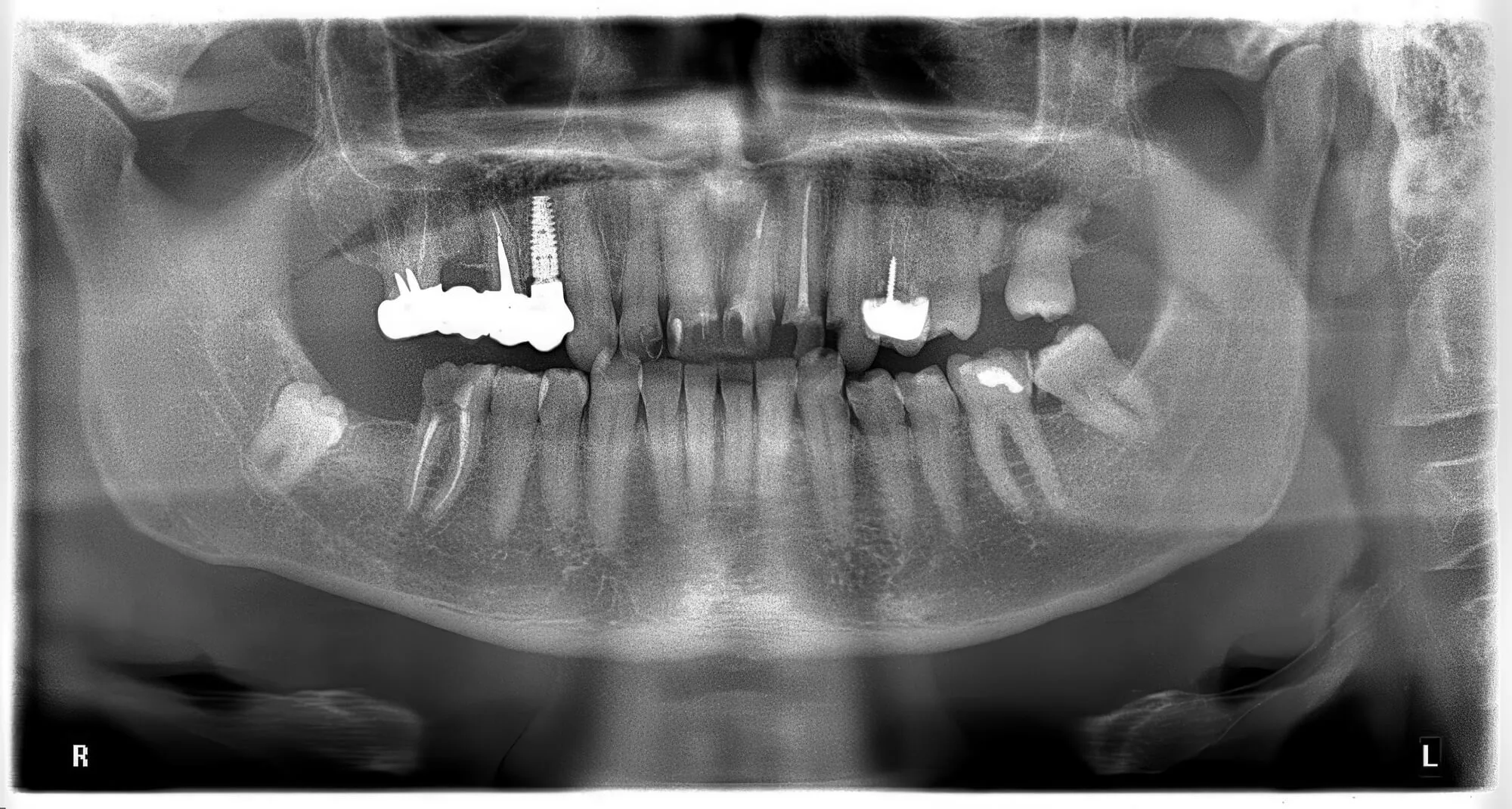
After losing a tooth, dental implants are one of the best restorative options available. Implants are as stable as a natural tooth, and that’s because they’re actually attached to your jawbone, offering unparalleled solidity and durability. However, good jawbone health is also necessary before starting the placement journey alongside a Chicago implant dentist.
Good jawbone health means successful osseointegration, a process in which the titanium post “blends in” with your bone to remain stable no matter what foods you eat. But what does this process involve—and what considerations should you keep to ensure its success?
What Is Osseointegration—And How Does It Impact Implant Dentistry?
Osseointegration is the biological fusion between your living jawbone and the surface of a dental implant. Coined by Swedish orthopedic surgeon Per-Ingvar Brånemark in the 1960s, it makes modern dental implants a long-term, stable replacement for natural teeth.
The secret to osseointegration success is that bone and the surface of an implant make a direct structural and functional connection. This means no fibrous tissue forms between the implant and the bone, resulting in a better attachment and long-term stability.
Osseointegration occurs as follows:
- Immediately after implant placement, blood clots form around the implant.
- Mesenchymal stem cells (MSCs) are recruited to the implant site, where they differentiate into osteoblasts—the bone-forming cells. Osteoblasts start laying down bone matrix on and around the implant surface.
Eventually, the implant is firmly anchored by newly formed bone, integrating it into the jaw's functional load-bearing structure.
The Importance of Osseointegration for Long-Term Implant Success
Since osseointegration provides the biological and mechanical basis for a stable, functional, and long-lasting prosthetic tooth, it is absolutely essential for the long-term success of dental implants. Without proper osseointegration, an implant will fail, regardless of surgical precision or prosthetic design.
The importance of osseointegration can be assessed in more ways than one:
1. Stability Under Functional Load
Implants must withstand the forces of chewing, biting, and grinding—often up to hundreds of pounds of pressure. Osseointegration locks the implant into the bone, allowing it to function like a natural tooth root.
Without it, the implant will micromove, disrupting healing and leading to failure.
2. Prevention of Implant Mobility
Unlike natural teeth, implants have no periodontal ligament. Their stability depends entirely on the bone-implant interface.
Osseointegration ensures the implant is rigid and does not become loose or mobile, which would trigger peri-implantitis or bone loss.
3. Bone Preservation
Tooth loss leads to alveolar bone resorption over time due to insufficient stimulation. Osseointegrated implants stimulate the surrounding bone when loaded, helping to:
- Maintain bone volume
- Prevent facial collapse
- Preserve oral function and facial aesthetics
4. Barrier to Infection
A fully integrated implant acts as a seal against bacterial invasion. When osseointegration is poor or incomplete, gaps are left where biofilm and pathogens can colonize. This can cause soft tissue inflammation, increase the risk of peri-implantitis, and lead to progressive bone loss.
5. Longevity and Predictability
Studies have shown that dental implants have success rates above 95% over 10–15 years when osseointegration is successful.
Most implants can last decades or even a lifetime, so being careful during this process is key!
6. Foundation for Complex Restorations
Osseointegration is the bedrock for more advanced procedures:
- Full-arch restorations
- Implant-supported overdentures
- Zygomatic implants
These require multiple implants to be fully integrated to function as a single load-distributing unit.

Why Titanium Enables Osseointegration
Titanium is the gold standard for dental and orthopedic implants due to its exceptional biocompatibility. One of the reasons why is that, within nanoseconds of exposure to oxygen, titanium spontaneously forms a thin, stable, and inert layer of titanium dioxide (TiO₂) on its surface. This oxide layer:
- Prevents corrosion in the harsh, moist oral environment.
- Reduces immune response, so the body doesn't recognize it as a foreign object.
- Acts as a biological scaffold for protein adsorption and bone cell attachment.
Moreover, titanium has a high strength-to-weight ratio and has an elastic modulus closer to bone than other metals like stainless steel. This helps transfer functional loads to the surrounding bone without causing stress shielding, promoting bone maintenance and remodeling.
The best part? Titanium is non-magnetic, meaning you don’t have to worry about attracting metals with your new smile!
Are There Alternatives to Titanium?
Nowadays, zirconia implants have emerged as a reliable alternative for patients with metal allergies or autoimmune sensitivities or who want to avoid titanium overall.
Unlike titanium implants, which are divided into three elements, zirconia implants are placed as a single restoration. For that reason, patients leave the dental office with a complete, brand-new restoration.
Zirconia is highly natural-looking, and there’s no risk of a grey implant showing through. Additionally, the material has low plaque affinity, which means fewer bacteria could cause peri-implantitis around your implant.
The Problem of Zirconia Implants
However, zirconia doesn’t perform quite as well as titanium. Zirconia also forms an oxide layer (ZrO₂), but the biological interaction differs. Early studies showed slightly lower bone-to-implant contact (BIC) than titanium, especially in early healing.
Newer surface treatments (like sandblasting or laser microgrooving) have improved zirconia's osseointegration capabilities. However, the biggest issue with this new material is that there is simply not as much reliable long-term data.
Dentists have been placing dental implants since 1965, which means there are 60 years of studies about their effectiveness and long-term success. Zirconia implants started being placed in the 2000s, so think of them as a young, more inexperienced 25-year-old.
What Can I Do to Ensure a Smooth Osseointegration Process?
Whether you’ve just had a dental implant placed or are preparing for the procedure, your actions during the healing period are critical to ensure the implant fuses with your bone properly. To do so, you can:
- Follow your dentist’s instructions, including medications, oral care routines, and post-op restrictions. If antibiotics are prescribed, complete the full course.
- Don’t smoke. Smoking significantly reduces blood flow and oxygen to the bone, which is why it is one of the leading causes of implant failure.
- Keep the area clean, using any prescribed antibacterial mouth rinses like chlorhexidine.
- Keep a soft diet, avoiding hard or crunchy foods.
- Rest and take it easy. Avoid strenuous exercise, heavy lifting, or bending over for at least 48–72 hours after surgery.

Ensure a Successful Osseointegration With a Knowledgeable Chicago Implant Dentist
Osseointegration has revolutionized restorative dentistry by enabling the development of fixed, long-lasting prosthetics that mimic the function and aesthetics of natural teeth. Besides ensuring a successful single implant, it opened the door to more complex and complete procedures like full-mouth restorations and All-on-4®.
While your oral surgeon will probably help you prepare for this procedure, you can feel better prepared by following these tips and understanding how the process goes. If you have any questions, you can contact 3020 Dental Implants! We’re committed to ensuring you know what’s happening every step of the implant process.
"Nobel Biocare, NobelProcera, NobelGuide and All-on-4 are trademarks of the Nobel Biocare group."